6 Innovations in Obesity Surgery: What’s New in the Field?:
Obesity surgery, or bariatric surgery, has come a long way over the years, continually evolving to offer more effective, safer, and less invasive options for those struggling with severe obesity. The latest advancements are reshaping the landscape of weight loss surgery, offering hope and improved outcomes for patients worldwide. In this comprehensive guide, we’ll explore the latest innovations in obesity surgery, focusing on two popular procedures: sleeve gastrectomy and gastric bypass. We’ll also discuss how changing your lifestyle with weight loss surgery can lead to lasting success.
1. Innovations in Sleeve Gastrectomy
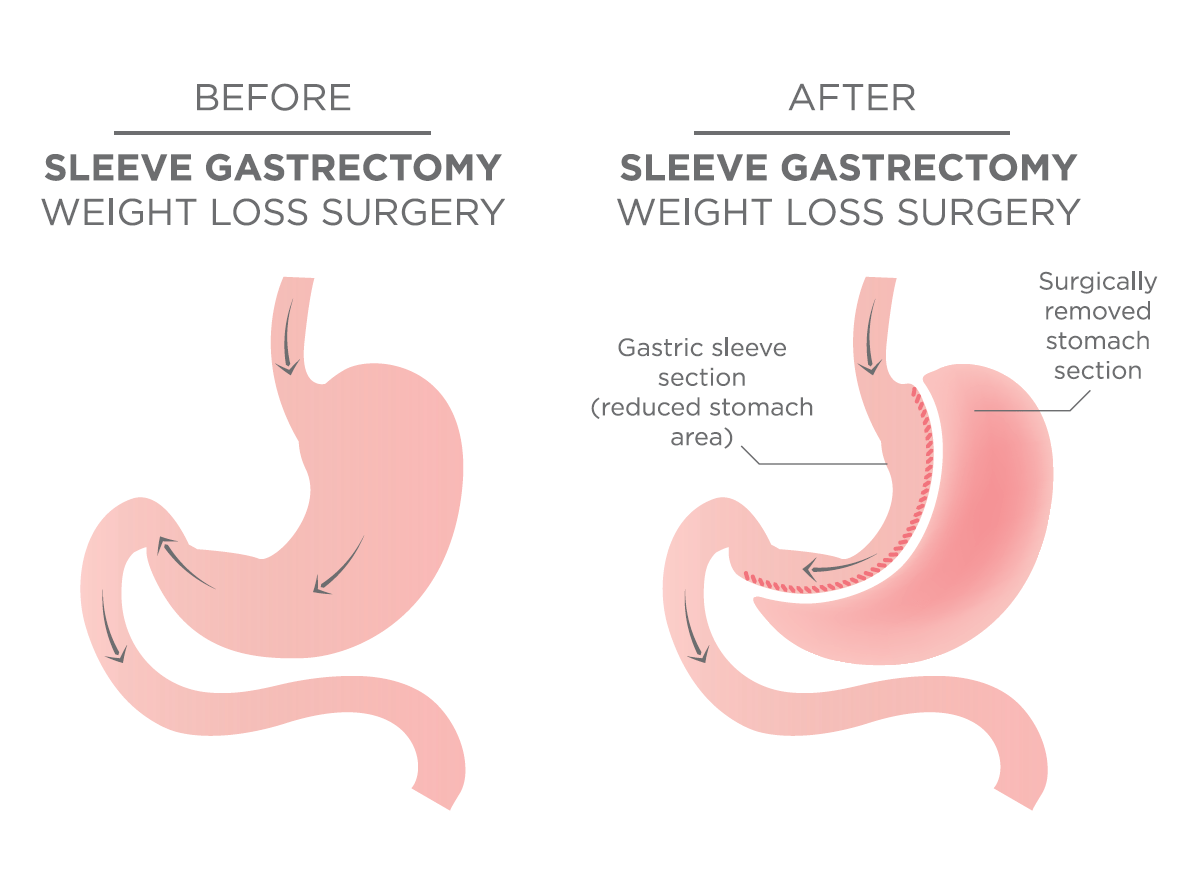
What is Sleeve Gastrectomy?
Sleeve gastrectomy, also known as vertical sleeve gastrectomy (VSG), is a weight loss surgery that involves removing a significant portion of the stomach, leaving behind a small, tube-like stomach. This procedure limits food intake and helps patients feel full more quickly. Recent advancements have made this surgery safer, more precise, and more effective.
Minimally Invasive Techniques
Laparoscopic Surgery
Traditional sleeve gastrectomy was performed through a large incision, which could lead to longer recovery times and more significant scarring. The introduction of laparoscopic techniques has transformed this approach:
- Enhanced Visualization: Modern laparoscopic equipment includes high-definition cameras and advanced imaging tools that provide surgeons with a detailed view of the surgical area. This improved visualization allows for greater precision in making incisions and performing the procedure.
- Advanced Instruments: Newer laparoscopic instruments are more flexible and easier to maneuver within the abdominal cavity. This helps in reducing the risk of complications and improves the overall effectiveness of the surgery.
Robotic-Assisted Surgery
Robotic systems have further refined laparoscopic techniques. These systems offer:
- Precision and Control: Robotic-assisted surgery allows for greater precision and control during the operation. Surgeons use robotic arms equipped with high-definition cameras and specialized instruments to perform the surgery through small incisions.
- Enhanced Dexterity: The robotic systems provide enhanced dexterity, making complex maneuvers easier and reducing the risk of errors.
Personalized Surgical Approaches
Tailored Surgical Plans
Advances in pre-operative assessment and planning have led to more personalized approaches to sleeve gastrectomy:
- 3D Imaging: High-resolution 3D imaging provides detailed views of a patient’s anatomy, enabling surgeons to plan the surgery with greater accuracy. This technology helps in making precise adjustments and reduces the likelihood of complications.
- Customized Techniques: Surgeons can now tailor the sleeve gastrectomy technique to fit an individual’s specific anatomy and needs, improving outcomes and minimizing risks.
Innovations in Post-Operative Care
Enhanced Recovery Protocols
Post-operative care has seen significant improvements, focusing on reducing recovery times and managing complications more effectively:
- Enhanced Recovery After Surgery (ERAS) Protocols: These protocols are designed to promote quicker recovery by minimizing the impact of surgery on the body. They include strategies such as pain management, early mobilization, and optimal nutrition.
- Advanced Pain Management: New techniques in pain management, including targeted nerve blocks and advanced pain medications, help in reducing post-operative discomfort and facilitating faster recovery.
2. Innovations in Gastric Bypass Surgery
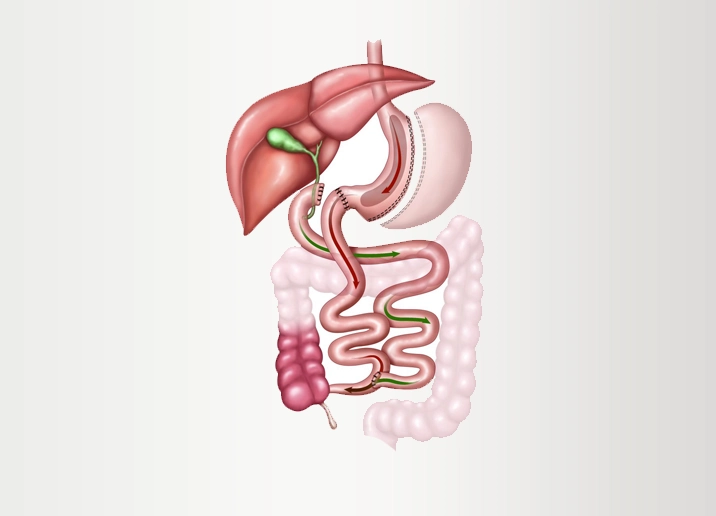
What is Gastric Bypass?
Gastric bypass, or Roux-en-Y gastric bypass (RYGB), is a weight loss surgery that creates a small stomach pouch and reroutes a portion of the small intestine to this pouch. This reduces the amount of food that can be eaten and limits the absorption of nutrients. Recent innovations have made this procedure more effective and safer.
Minimally Invasive Techniques
Robotic-Assisted Surgery
Similar to sleeve gastrectomy, gastric bypass has benefited from robotic-assisted surgery:
- Increased Precision: Robotic systems offer precise control and high-definition visualization, allowing for more accurate placement of the stomach pouch and bypass.
- Reduced Complications: The improved dexterity and control provided by robotic systems help in minimizing complications such as leakage and infection.
Advanced Laparoscopic Tools
Recent advancements in laparoscopic tools have improved the performance of gastric bypass surgery:
- Improved Visualization: Enhanced cameras and imaging systems provide better views of the surgical field, helping surgeons make more precise incisions and adjustments.
- Innovative Instruments: New laparoscopic instruments are designed to handle complex tasks with greater ease, improving the overall efficiency of the procedure.
Enhanced Surgical Outcomes
Refined Anastomosis Techniques
Anastomosis, the connection between the stomach pouch and intestines, is a critical aspect of gastric bypass surgery. Innovations in this area include:
- Advanced Techniques: New methods for creating and securing anastomoses reduce the risk of leakage and other complications. These techniques improve the overall safety and effectiveness of the surgery.
- Real-Time Imaging: The use of real-time imaging during surgery helps in ensuring accurate placement of the anastomoses, further reducing the risk of complications.
Post-Operative Care Innovations
Comprehensive Support Programs
Post-operative care for gastric bypass patients has evolved to include more comprehensive support:
- Personalized Nutritional Counseling: Customized nutritional plans are designed to meet the specific needs of patients, focusing on balanced diets and addressing potential deficiencies.
- Behavioral Therapy and Lifestyle Coaching: Programs that include behavioral therapy and lifestyle coaching support patients in making long-term changes that promote sustained weight loss and overall health.
3. The Role of Technology in Obesity Surgery
Telemedicine and Remote Monitoring
Telemedicine
The integration of telemedicine into obesity surgery has enhanced patient care and accessibility:
- Virtual Consultations: Patients can now have pre-operative and post-operative consultations via video calls. This convenience helps in managing care from home and reduces the need for frequent in-person visits.
- Remote Monitoring: Wearable devices and mobile apps track important health metrics, such as weight, activity levels, and dietary intake. This data allows healthcare providers to monitor progress and make timely interventions.
Advanced Imaging and Diagnostic Tools
Cutting-Edge Imaging Technologies
Advancements in imaging technologies play a crucial role in obesity surgery:
- High-Resolution Scanning: New imaging techniques, such as high-resolution CT and MRI scans, provide detailed images of the anatomy, assisting in precise surgical planning.
- Real-Time Imaging: Real-time imaging during surgery enhances the surgeon’s ability to make informed decisions and ensures optimal placement of surgical instruments.
4. Innovations in Minimally Invasive Techniques
Robotic-Assisted Surgery
Robotic Systems
Robotic-assisted surgery has become increasingly prevalent in obesity surgery, offering several advantages:
- Precision and Control: Robotic systems provide enhanced precision and control, allowing for complex procedures to be performed with smaller incisions and reduced risk.
- Improved Visualization: Robotic systems offer high-definition, 3D visualization of the surgical field, improving accuracy and outcomes.
Single-Incision Surgery
Single-Incision Techniques
Single-incision laparoscopic surgery (SILS) is an innovative approach that reduces the invasiveness of obesity surgery:
- Less Scarring: SILS involves performing the surgery through a single, small incision, which minimizes visible scarring and improves cosmetic results.
- Enhanced Recovery: With fewer incisions, patients often experience faster recovery times and reduced post-operative pain.
5. Advances in Pre-Operative and Post-Operative Care
Enhanced Pre-Operative Assessments
Comprehensive Evaluations
Recent advancements in pre-operative assessments help ensure better surgical outcomes:
- Detailed Risk Assessments: Improved tools and protocols for evaluating surgical risks aid in better planning and minimizing complications.
- Personalized Pre-Surgical Programs: Tailored programs focusing on nutrition, exercise, and mental health support prepare patients for surgery and enhance their ability to cope with post-operative changes.
Post-Operative Care Innovations
Advanced Recovery Strategies
New strategies in post-operative care focus on accelerating recovery and improving patient outcomes:
- Enhanced Recovery Protocols: These protocols, such as Enhanced Recovery After Surgery (ERAS), are designed to minimize the impact of surgery on the body and promote quicker recovery through strategies like optimized pain management and early mobilization.
- Long-Term Support: Ongoing support through follow-up appointments, nutritional counseling, and lifestyle coaching helps ensure that patients maintain weight loss and overall health in the long term.
6. Changing Your Lifestyle with Weight Loss Surgery
Adopting a New Lifestyle
Lifestyle Changes Post-Surgery
Changing your lifestyle with weight loss surgery involves significant adjustments to ensure long-term success:
- Dietary Adjustments: After surgery, patients need to adopt a balanced, nutrient-dense diet. Post-surgery dietary plans often emphasize high-protein foods, fruits, vegetables, and whole grains while limiting high-calorie, low-nutrient foods.
- Regular Exercise: Incorporating physical activity into your daily routine is crucial for supporting weight management and improving overall fitness.
- Behavioral Changes: Addressing emotional and behavioral factors related to eating can enhance the effectiveness of the surgery and support long-term success.
Support and Resources
Utilizing Support Systems
Effective weight loss and lifestyle changes are supported by various resources:
- Support Groups: Joining support groups provides motivation, shared experiences, and practical advice from others who have undergone similar procedures.
- Healthcare Providers: Regular consultations with healthcare providers ensure ongoing monitoring, adjustments to dietary plans, and management of any post-surgical issues.
Conclusion:6 Innovations in Obesity Surgery: What’s New in the Field?
The field of obesity surgery has seen remarkable innovations that enhance both the surgical experience and patient outcomes. Advancements such as minimally invasive techniques, robotic-assisted surgery, and enhanced pre- and post-operative care are improving the effectiveness, safety, and overall experience of weight loss surgery.
Changing your lifestyle with weight loss surgery involves adopting new dietary habits, increasing physical activity, and addressing emotional factors. Embracing these changes, supported by the latest innovations in bariatric surgery, can lead to long-term success and improved quality of life.